Dr Gautam Tawari is an accredited orthopedic sports surgeon from The Royal College of Surgeon in the UK. Now practicing as a Othoprdic Doctor in Mumbai. He has a Diploma in Sports & exercises Medicine (Dip.SEM) from the college and is a Fellow of the Sports & Exercise Medicine Society of the UK.
He is a fellowship trained Orhtopedic hand surgeon from the UK & has worked as a Consultant Orthopaedic Surgeon in the UK. He specialises in advanced hand surgery and Sports related injuries to the hand and fingers.
The common sports related injuries he treats surgically include – Hand fractures / trauma and finger fractures, Finger ligament reconstruction and repairs, Tendon injuries, Thumb ligament repairs & reconstruction.
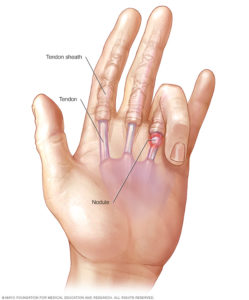
Fingers can bend due to action of tendons, these tendons are supported along their length by tunnels of ligaments called pulleys. Inflammation of this tendon sheath (teno-synovium) leads to snapping when the finger is straightened, this is called trigger finger or trigger thumb.
Cause
- Inflammation
- Presence of nodule
- Repetitive Motion – Individuals who perform heavy, repetitive hand and wrist movements or prolonged gripping.
- Medical Conditions – Hypothyroidism, Rheumatoid arthritis, diabetes, and sometimes Tuberculosis.
Presentation
- Pain and tenderness over inflamed tendon nodule.
- Sudden popping sensation and straightening of finger.
- Feeling of stiffness in finger joints.
- Locking with inability to straighten the finger/thumb.
Long-term complications of untreated trigger finger/thumb can include permanent digital swelling and joint stiffness or tearing of the tendon.
Treatment
Non surgical treatment is used in early stages of the condition. This includes :-
- Activity modification – Rest, avoiding repetitive gripping actions.
- Occupational therapy – massage, heat, exercises to improve the finger movements.
- Non-steroidal anti-inflammatory drugs (NSAIDs) may help to relieve pain and inflammation.
- Steroid injections may help reduce the inflammation.
Surgery is advocated in case of nodule, late stage of condition on presentation, recurrence or failure of non-surgical treatment.
Trigger finger/Thumb release surgery is performed under local anaesthesia or Wrist Block. The pulley resulting in tightness is released to allow free movement of the tendon. Recovery takes 2 weeks after surgery, residual stiffness may take unto 3 months to settle fully.
Tendon lacerations can lead to permanent disability, these injuries need to be diagnosed and treated early with proper follow-up arrangements.
All hand lacerations (cuts) should be explored to confirm injuries to joint, bone, nerve, tendon, or vascular injury.
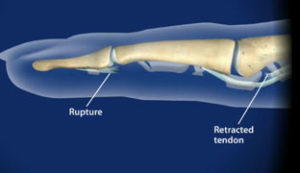
- Flexor Tendon Injuries
Flexor tendon injuries are divided into five zones, and are often associated with joint, nerve, or vascular injury.
Flexor zone II injuries are the most complex tendon injuries with variable outcome to repair. The other zonal repair do well with primary repair. It is recommended that all flexor tendon injuries should be repaired by a hand surgeon, owing to the high rate of complications that can occur even after an optimal repair.
Rehabilitation
Following repair, it is paramount to undergo physiotherapy as advised. Delayed or non compliance in physiotherapy has a poor outcome following repair.
- Extensor Tendon Injuries
Extensor tendon injuries are divided into eight zones. These tendon fibers are thin and flat that do not hold sutures well, therefore, it is recommended that a hand surgeon undertakes the repairs. Following the repair, rehabilitation is paramount with the help of physiotherapy to achieve optimal movement of the fingers.
- Rupture of the Central Slip
Central slip is a structure of extensor tendon complex at the PIP joint. It is a common sports injury and typically rupture following forced flexion of the PIP joint or dislocation of the PIP joint. This often results in a boutonniere deformity.
Presentation
- Swelling of the PIP joint over its dorsal surface.
- Limited extension at the PIP joint, with hyperextension of the DIP joint.
Treatment
Initial treatment requires splinting of PIP joint, chronic deformity requires reconstruction of the Central Slip with surgical procedure.
- Extensor Hood Rupture
Extensor hood is a tissue structure that allows in line position of the tendon with the MCP joints are extended. Rupture commonly due to blunt trauma and results in subluxation of the central tendon, preventing full extension.
Presentation
The middle (long, third) fingers is most commonly affected, followed by the index (second) finger. Pain overlying the MCP joint with loss of full extension at the MCP joint. Popping sensation or/and instability of the MCP joint when it is actively flexed and extended.
Treatment
Extensor hood injuries require surgical repair/reconstruction and is associated with a favorable functional outcome and decreased pain.

Ulnar Collateral Ligament is an important stabilising ligament of the MP joint of the thumb. Rupture of the ulnar collateral ligament (UCL), also known as “gamekeeper’s thumb” is a sports injury commonly seen with skiing, basketball, wrestling, and martial arts.
Presentation
Painful swollen thumb that is tender over the ulnar side of the MCP joint. May be associated with instability with use of thumb. The finger may be deviated radially.
Treatment
Acute UCL injuries are treated with a thumb spica splint or custom splinting to maximize functional outcomes and prevent long-term disability.
Rupture of the ligament requires surgical repair or reconstruction and should be undertaken preferably by hand surgeon only.
Mallet finger is a flexion (bent) deformity at the end joint of the finger. It usually results from a direct blow to the fingertip which causes disruption of the extensor tendon as it inserts into the base of the distal phalanx. Occasionally, an avulsion fracture / trauma of the base of the distal phalanx can be seen on radiographs.
Presentation
Pain at the base of the distal phalanx (End bone of the finger)
Inability to extend (straighten) the fingertip fully
Permanent flexion of the fingertip may lead to a swan-neck deformity
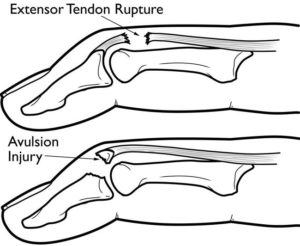
Treatment
Initial treatment is with a mallet finger splint with the distal interphalangeal (DIP) joint in full extension for 8 weeks. Despite adequate splintage, there can still be some bend at the finger tip.
Surgery is advocated if a bony avulsion (fragment) is present or on failure of non surgical treatment. Reconstruction surgery for mallet finger deformity has an average to good outcome, hence should be advocated cautiously.